In 2021, there were over 71,000 opioid overdose deaths in the U.S. Opioids have a powerful effect on the brain and body. They block pain sensations, lower body temperature and even slow heart rate and respiration functions. Anyone who takes opioids — prescribed or illicit — risks these effects, along with overdose.
Millions of Americans struggle with opioid use disorder (OUD), making it essential to learn how to spot signs of an overdose and how to prevent one. If you or someone you know is struggling with OUD, continue reading to learn what happens during an overdose and how to get treatment.
How to Recognize an Overdose
An overdose can occur when a person takes too much of an opioid or combines it with other substances at a level that is toxic to the body. Sometimes, it can be challenging to recognize when a person is experiencing a life-threatening overdose. If you are unsure, it’s best to assume that it is an overdose and seek help immediately. Signs of an opioid overdose include:
- Cold or clammy skin
- Restricted or stopped breathing
- Seizure
- Slow or irregular heartbeat
- Snoring or gurgling sounds
- Discolored lips or fingernails
- Nausea and vomiting
- A rapid change in body temperature
- Chest pain
- Constricted pupils
- Unresponsiveness or unconsciousness
Seek emergency health services immediately if you or someone you know experiences these symptoms. Overdoses can be fatal if neglected. It is one of the most dangerous outcomes of OUD, killing more than 136 Americans daily.
Overdose can occur from a person taking too much of a substance. However, the risk increases when someone combines opioids with other depressants, like benzodiazepines and alcohol. The combination can intensify the effects of the opioid, raising the levels of narcotics in the body. In 2017, synthetic opioids contributed to the country’s highest rate of alcohol-induced overdoses.
Fentanyl is a synthetic opioid that is 100 times stronger than morphine. Many illicit substances are laced with fentanyl, contributing to the high opioid deaths we see today.
What Happens When You Overdose?
Opioids work by depressing the central nervous system, slowing our functions and movements. The central nervous system is responsible for heart rate, breathing and other crucial bodily functions. Opioid overdose death can occur when the substance overwhelms the brain and interrupts the body’s natural drive to breathe. That’s why you may notice symptoms such as blue or purple fingernails and lips when a person is experiencing an overdose. They may also become limp, pale or unresponsive.
Combining opioids with sedating substances like alcohol can increase the risk of overdose. The combination can intensify side effects like sedation, slowed breathing and drowsiness. These overdose symptoms can even cause brain damage by reducing the amount of oxygen getting to the brain.
Opioids contain chemicals that bond with opiate receptors in the brain, causing pain-relieving effects when prescribed legally. However, when taken illicitly or in excess amounts not prescribed by a health provider, opioids can cause euphoria, triggering a response from the pleasure and reward pathways of the brain. This effect can lead to addiction and increase a person’s chances of experiencing an overdose.
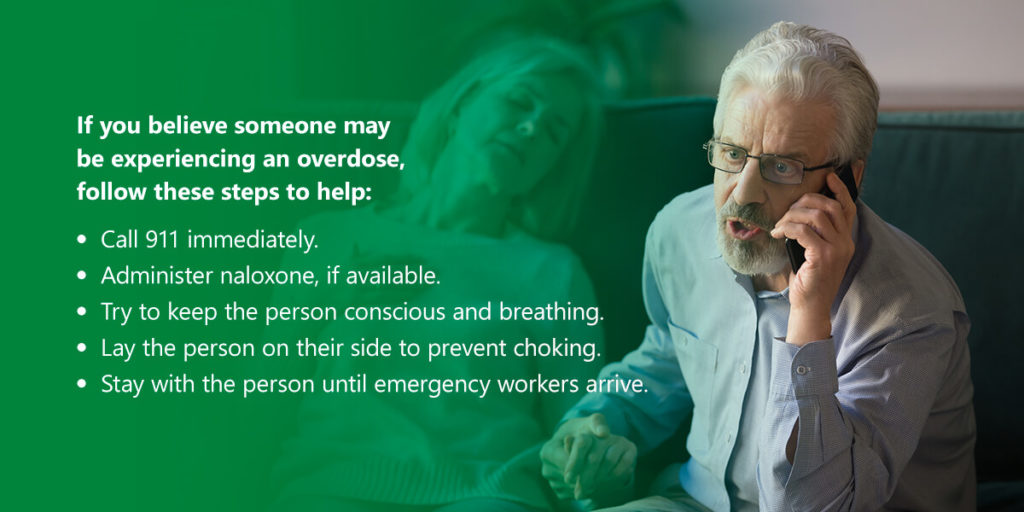
How to Prevent and Respond to an Overdose
It’s crucial to know how to prevent and respond to an opioid overdose to avoid its adverse effects. If you believe someone may be experiencing an overdose, follow these steps to help:
- Call 911 immediately.
- Administer naloxone, if available.
- Try to keep the person conscious and breathing.
- Lay the person on their side to prevent choking.
- Stay with the person until emergency workers arrive.
If prescribed opioids, you can prevent an overdose by following these steps:
- Start a conversation with your doctor: Know the risks of opioid addiction and overdose when taking prescribed medicine. Ensure that what you get is safe, effective and right for you. Also, remember to let your doctor know if you have any side effects or concerns.
- Only take opioids as directed by a doctor: Do not take prescription opioids in more significant amounts or more than prescribed.
- Never combine opioids with other substances: Do not take opioids with alcohol or other substances. These include benzodiazepines, muscle relaxants, hypnotics or other prescription opioids. Doing so can lead to an overdose caused by elevated levels of narcotics in the body.
Do not share or sell prescription opioids: Always keep prescription medicines in a safe and secure place. Store opioids in a locked space, such as a key cabinet or drawer, to keep them away from children, friends, family and visitors. - Properly discard unused or expired prescription opioids: When you are finished with your course of pain relievers, remove them from your home as soon as possible to reduce the chances of misuse.
- Seek professional treatment: An addiction care center can help you or a loved one struggling with opioid addiction reduce the chance of an overdose and other adverse outcomes.
When to Seek Professional Addiction Treatment
When a person struggles with an addiction to opioids, stopping can become more challenging. Their reliance can interfere with their daily routines and relationships and have serious health complications, including an overdose. While a complex disease, opioid addiction is also treatable.
You should seek professional OUD treatment if you:
- Take opioids longer or in more significant amounts than prescribed.
- Attempted to cut back opioid use unsuccessfully.
- Spend time frequently taking, finding or recovering from opioids.
- Experience cravings to take substances.
- Realize that your substance use interferes with your work, school or home life.
- Continue using the substance even when it causes relationship issues.
- Use the substance in situations where it’s physically dangerous to do so.
- Need more of the opioid to create the desired effect.
- Find it challenging to quit the substance on your own.
Medication-assisted treatment (MAT) can treat addiction and prevent opioid overdose. These programs utilize medications alongside counseling to provide a whole-patient approach to treating OUD. All medications are FDA-approved, and health providers design MAT programs to meet each patient’s unique needs.
Research shows this approach can effectively treat addiction and help sustain recovery. These programs may also prevent or reduce opioid overdoses, making them crucial if you or someone you know is struggling. Medicines can help balance brain chemistry, block the euphoric effects of opioids and relieve withdrawal symptoms to ease patients through recovery.
Receive Professional Opioid Addiction Treatment
While complex and chronic, OUD is a disease that can be treated. If you or a loved one is struggling with opioid addiction, Health Care Resource Centers can help. Our health providers will design an individualized treatment program that works for you. Counseling and FDA-approved medicines can help you throughout recovery.
It’s important that you know you are never alone in your recovery journey. Get in touch with us today to learn how our programs can help.