According to the National Survey on Drug Use and Health (NSDUH), an estimated 2.1 million people had an opioid use disorder (OUD) in 2016. The majority of people with OUD had an addiction to prescription pain pills. Over half a million people had an addiction to heroin. Every day, more than 130 people die in the United States after overdosing on opioids such as prescription pain relievers and heroin.
OUD is a complex condition, but it’s also treatable. Medication-assisted treatment (MAT) is an effective treatment for people with OUD. MAT involves the combination of medication, individual counseling and group counseling. Suboxone may be the medication used in MAT.
Suboxone® is a relatively new medication used to help individuals recover from OUD. Suboxone has been found to be an effective medication for those in MAT. However, some people, particularly those who did not previously have OUD, abuse Suboxone to get high. Those with OUD may attempt to use Suboxone to experience euphoric feelings. Suboxone is a controlled substance which carries the risk of addiction and dependence.
[maxbutton id=”2″ text=”Find A Treatment Center Near You” url=”https://www.hcrcenters.com/our-location/”]
If you or a loved one struggle with OUD and Suboxone use or have questions about this medication, we hope to help. In this post, we aim to answer common questions about Suboxone and how it can help those with OUD, but also potentially lead to opioid addiction.
What Is Suboxone®?
Suboxone is the brand name of a medication which combines buprenorphine and naloxone. Buprenorphine is a type of medicine called a partial opioid agonist. This means that buprenorphine activates the same opioid receptors in the brain as full agonists such as methadone or heroin, but does not activate the receptors as strongly. As a result, buprenorphine produces a lower degree of sedation and respiratory depression than full agonists, and does not impair cognitive or motor skills. It tricks the brain into thinking it is receiving a strong opioid which keeps withdrawal symptoms away. A person with OUD will feel “normal” after taking buprenorphine once a therapeutic dose is reached.
Naloxone is an opioid antagonist. This means it blocks the activation of opioid receptors. After taking naloxone, a person will not feel euphoria from an opioid. Naloxone reverses euphoric effects, but also causes immediate withdrawal symptoms when used improperly. By combining both buprenorphine and naloxone, Suboxone is meant to reduce withdrawal symptoms and deter misuse.
Suboxone comes in the form of a sublingual film which is taken and dissolved under the tongue usually once a day. A doctor may start a patient on a low dose of buprenorphine before switching to Suboxone. Sometimes a doctor will start a patient on Suboxone right away depending on the type of opioid they were taking. Patients are told to take Suboxone exactly as directed.
What Is Suboxone® Used For?
Doctors may prescribe Suboxone as part of treatment for OUD. It is effective in treating an addiction to heroin, as well as an addiction to any type of opiates such as OxyContin or Percocet. Suboxone, along with counseling, has been proven to successfully treat OUD and help people maintain recovery.
For example, according to a study conducted by the National Institute on Drug Abuse (NIDA), half of the study participants reduced painkiller misuse during extended Suboxone treatment. After three and a half years, 61 percent reported being abstinent from opioid pain relievers, and less than 10 percent met the criteria for dependence on drugs.
When used as part of MAT, the goal of Suboxone administration is a complete recovery. MAT has been shown to improve patient survival, decrease illicit opiate use, increase retention in a treatment program, and increase the chance of gaining and maintaining employment. It is the most effective intervention to treat OUD and is more effective than using only behavioral or medication therapy alone.
Medications such as Suboxone do not replace an opioid addiction with a new addiction. Doctors monitor patients who receive medication as part of treatment and give them an amount that does not get them high but reduces cravings. It helps the patient return to a balanced condition so they can heal while they recover.
Suboxone® vs. Methadone
You may be wondering how Suboxone differs from methadone – another commonly used medication for OUD treatment. According to a review published in the Journal of Addiction Research and Therapy, both Suboxone and methadone are proven to be effective treatment options for opioid addiction recovery. They both have advantages and disadvantages, and neither is better than the other. Whether or not a patient should take Suboxone or methadone depends on their unique needs. A doctor must evaluate a patient and consider factors such as dosing schedule, side effects, risk of misuse and cost.
Perhaps the most significant difference between Suboxone and methadone is the risk of misuse. Methadone is a full agonist opioid, which means it produces stronger feelings of euphoria than Suboxone. It is also an effective pain reliever for patients with chronic pain. Suboxone, on the other hand, is less likely to be misused because it is a partial agonist. The naloxone in Suboxone prevents the drug from producing intoxicating effects if it is diluted and injected and can initiate withdrawal symptoms instead. Therefore, patients are also less likely to inject Suboxone. The risk of overdosing on methadone is higher than Suboxone.
Despite the risks, methadone may be a more effective treatment option for patients with high levels of physical dependence on opioids. Suboxone may not be sufficient for helping some patients maintain treatment therapy. Generally, Suboxone is best for patients addicted to a lower opiate dose or who do not have access to treatment facilities. Suboxone can be prescribed by a local doctor, which makes it more convenient for people who live in rural communities.
There are many more studies about methadone and its long-term effects because it has been used in treatment much longer than Suboxone. Suboxone did not receive approval by the Food and Drug Administration (FDA) until 2002. The FDA approved methadone for addiction treatment in 1972. Even though Suboxone is a new medication compared to methadone, the number of treatment programs offering Suboxone is increasing. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), the number of opioid treatment programs (OTPs) offering buprenorphine products such as Suboxone increased from 11 percent in 2003 to 58 percent in 2015.
Does Suboxone® Get You High?
Patients might wonder if they can get high on Suboxone strips. The answer to this question depends on the person. Patients with OUD cannot get high on Suboxone if they take the medication as prescribed by their doctor. However, a patient can get intoxicated if they combine Suboxone with other substances or do not take it as directed. People who do not have OUD may become intoxicated from taking Suboxone.
Buprenorphine has a “ceiling effect,” which means that a higher dose does not produce increased effects after a certain point. If a patient with OUD takes too much Suboxone, they will experience withdrawal symptoms rather than any pleasurable effects. For example, a study published in 2008 found that out of five patients who misused Suboxone intravenously, all reported that injecting Suboxone felt like “nothing” regarding euphoria or that is was a negative experience. For this reason, Suboxone is less likely to be misused than other opiates by patients with OUD.
Suboxone Abuse: Using Suboxone® to Get High
Even though Suboxone is weaker than other opiates, it’s still a partial agonist and can produce an opioid effect. The Drug Enforcement Administration (DEA) lists buprenorphine products such as Suboxone as a Schedule lll drug. This means it’s a controlled substance with low to moderate potential for physical and psychological dependence. In other words, people who misuse Suboxone can also become addicted to it.
People may snort or inject Suboxone to get high. Law enforcement reports show that Suboxone is successfully misused by snorting the drug. People who are not in addiction treatment programs may obtain Suboxone from patients who sell or give their medication away. For example, according to the National Drug and Intelligence Center, Suboxone is being diverted and sold primarily in the Northeast region of the country. Some people buy Suboxone illegally to treat their addiction themselves and keep withdrawal symptoms at bay – not to get high.
People may use Suboxone with alcohol or other opiates to get high. Using Suboxone with heroin does not increase the effects, but using it with methadone enhances the effects of both. Taking Suboxone with other substances increases the risk of overdose death.
Who Would Use Suboxone® to Get High?
Suboxone is more likely to be misused by individuals who are addicted to a low dosage of opiates or who are in the beginning stages of opiate addiction since a high dose can cause withdrawal symptoms. People with a high tolerance to opiates might try to misuse Suboxone to experience the euphoric effects of drugs like heroin or morphine.
If you or someone you love uses Suboxone to get high, know that help is available to you. Opioid addiction is a disease, like cancer or diabetes. However, it is a treatable disease and individuals can recover from opioid addiction. MAT programs help people address addiction as a whole, treating underlying mental health issues and addressing physical dependence. For patients who are already in recovery, a MAT program can help keep them on track and avoid misusing Suboxone.
Side Effects, Withdrawal and Overdose of Suboxone®
Like any medication, patients may experience certain side effects with Suboxone when they take it as directed. People who misuse Suboxone may also experience side effects. Patients can discuss their concerns about medication with their doctor. A doctor is there to help patients find the right dose for their unique situation. If you use Suboxone under a doctor’s guidance, you should always let them know if you experience anything unusual. If you misuse Suboxone, consider seeking treatment today. Suboxone can be deadly if misused.
1. Suboxone® Side Effects
Patients taking Suboxone may experience any of the following common side effects. If you experience side effects that make you uncomfortable or do not go away, speak with your doctor.
- Nausea
- Vomiting
- Headache
- Sweating
- Mouth numbness
- Constipation
- Swollen or painful tongue
- Lightheadedness
- Heart palpitations
- Blurred vision
- Back pain
- Fainting
- Dizziness
- Sleep issues
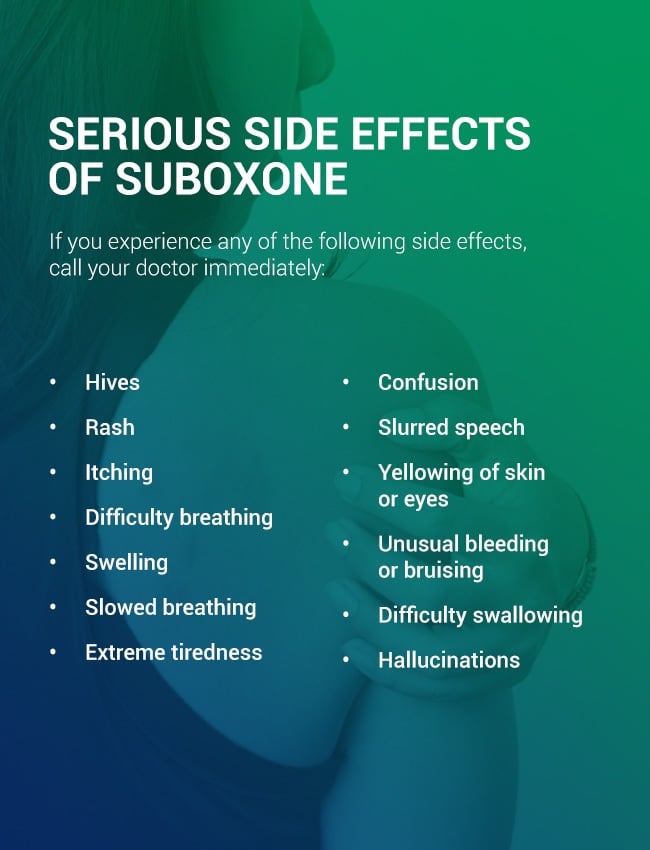
2. Serious Side Effects
Some people may experience serious side effects when they take Suboxone. If you experience any of the following side effects, call your doctor immediately:
- Hives
- Rash
- Itching
- Difficulty breathing
- Swelling
- Slowed breathing
- Extreme tiredness
- Confusion
- Slurred speech
- Yellowing of skin or eyes
- Unusual bleeding or bruising
- Difficulty swallowing
- Hallucinations
Even if a side effect is not on the list, let your doctor know right away if you experience something out of the ordinary when taking Suboxone.
3. Signs and Symptoms of Suboxone® Misuse
If you suspect that a loved one is misusing Suboxone, you can look for behavioral signs of opiate addiction, such as:
- Sudden mood swings
- Noticeable signs of euphoria
- Isolation
- Secrecy
- Legal issues
- Inability to fulfill commitments
- Issues with work, school, family or friends
- Sudden financial problems and the need for quick cash
- Changes in routines or habits
- Using more medication than prescribed
- Visiting multiple doctors to obtain more prescriptions for opioids
- An inability to stop using the drug
A Suboxone high may produce similar symptoms as any opiate. A person who is not used to opiates and takes too much Suboxone may feel relief from pain, calm and have a mild sense of euphoria. Someone who is addicted to Suboxone or another opioid may experience the following symptoms:
- Poor coordination
- Drowsiness
- Slowed breathing
- Nausea or vomiting
- Constipation
- Slurred speech
- Mood swings
- Irritability
- Depression
- Decreased motivation
- Anxiety attacks
- Change in sleep habits
4. Suboxone® Withdrawal Symptoms
If someone injects Suboxone, they face a risk of contracting a life-threatening disease or serious health issue. Also, taking Suboxone improperly can cause withdrawal symptoms in patients who are dependent on full agonist opioids such as morphine, methadone or heroin. Withdrawal symptoms associated with injecting Suboxone include:
- Muscle aches
- Cramps
- Vomiting
- Diarrhea
- Anxiety
- Sleep issues
- Cravings
- Shaking
- Sweating
Patients who take Suboxone for months or years to help them through recovery can experience withdrawal symptoms if they suddenly stop taking Suboxone. The buprenorphine in Suboxone is a long-acting agent, meaning some patients may not have to take a buprenorphine product every day. Long-acting opioid withdrawal symptoms usually emerge within 30 hours of the last exposure and may last up to 10 days. Although withdrawal symptoms are rarely life-threatening, they are still unpleasant. Withdrawal symptoms from stopping or dramatically reducing Suboxone may include:
- Muscle aches
- Runny nose
- Dilated pupils
- Agitation
- Anxiety
- Insomnia
- Yawning
- Abdominal cramping
- Nausea
- Vomiting
- Diarrhea
5. Signs of Suboxone® Overdose
It is possible to overdose on Suboxone if a person combines it with other drugs. The risk of overdose increases if Suboxone is taken with alcohol and other substances that depress the central nervous system such as benzodiazepines, sedatives, tranquilizers and antidepressants. The risk of an overdose is also higher for those who do not have a tolerance to opioids. Symptoms of a Suboxone overdose include:
- Pinpoint pupils
- Blurred vision
- Slowed breathing
- Dizziness
- Extreme drowsiness
If a loved one who is taking Suboxone collapses, has a seizure, has trouble breathing or cannot be awakened, call an emergency number for help immediately. Patients and people misusing Suboxone have a high risk of coma if they take Suboxone with medications like benzodiazepines.
Suboxone® Misuse Statistics
Although Suboxone can help people on the path to recovery from opioid addiction, it can be harmful to those who take Suboxone to get high. Suboxone has especially become a problem in American prisons. Smugglers send Suboxone to prisoners by turning it into a paste and spreading it over book pages, under stamps or tucking it behind envelope seams. Some prisoners with OUD may take Suboxone to stop withdrawal symptoms, while others may take Suboxone to get high. According to a New York Times article, Suboxone makes up 12 percent of all contraband discovered in state prisons in Massachusetts.
Suboxone misuse has also become an issue outside of prisons. For example, according to the Drug Abuse Warning Network, an estimated 21,483 emergency department visits were associated with the nonmedical use of buprenorphine in 2011 – almost five times the estimated number of buprenorphine visits in 2006. Similarly, the American Association of Poison Control Centers recorded 3,625 cases and three deaths involving buprenorphine in 2011.
Important Information About Suboxone®
Anyone who takes Suboxone should be aware of important information about the drug. Here are some points patients and users of Suboxone should keep in mind:
- Suboxone can cause serious breathing problems, and patients should call their doctor or get emergency help immediately if they feel faint, dizzy, confused or breathe more slowly than usual.
- Patients should not switch from Suboxone to other medicines containing buprenorphine without talking to a doctor first.
- Patients should speak with their doctor before they stop taking Suboxone to avoid discomfort.
- Suboxone is not meant to be taken “as needed.”
- Patients should always tell their doctor about other medications they take before they start taking Suboxone.
- People taking Suboxone should not drive or operate machinery until they know how it affects them.
- Suboxone can cause liver problems, and patients should tell their doctor if they have a history of liver or kidney issues.
- Some people might have an allergic reaction to Suboxone and should get help immediately if they experience a rash, hives, wheezing or swelling of the face.
- Suboxone may decrease fertility in men and women.
- Patients who are pregnant, plan to become pregnant or who are breastfeeding should talk to their doctor before taking Suboxone.
Other Forms of the Commonly Prescribed Drug Suboxone®
There is currently one other brand-name product containing both buprenorphine and naloxone – Zubsolv.
Zubsolv is a sublingual tablet. According to a review from 2018, Zubsolv has higher bioavailability, better taste and faster dissolve time than Suboxone. For these reasons, patients may prefer Zubsolv over Suboxone to help them overcome OUD.
Patients and people with OUD may expect to see generic Suboxone in the future. In June of 2018, the FDA announced they would take steps to promote the development of generic Suboxone to increase access to treatment for OUD.
Contact Health Care Resource Centers Today
Opioid addiction is heartbreaking, to both the person with the addiction and to loved ones. If you or a loved one is battling an opioid addiction, reach out to us at Health Care Resource Centers (HCRC). At HCRC, we are dedicated to delivering the highest quality care to those with an addiction to opioids. We have locations across New England and have been providing medication-assisted treatment for OUD for over 25 years. For more information, contact us today or find a treatment center near you.